3 Ways to Achieve Bunion Relief at Home
Tired of dealing with bunion pain? These bony bumps can sure…

Are Over-the-Counter Foot Peels Safe?
Calluses, cracks, dry skin—your feet can get pretty rough due…

It's Grass-Mowing Season: Use These Top Tips for Preventing Heel Pain
Springtime rolls around every year, and if you're using a push…

Am I at High Risk of Neuroma?
You may be at a higher risk for developing a neuroma if you frequently…

3 Chronic Diseases That Can Affect Your Feet
Many medical conditions can impact the health and function of…

Common Myths About Neuroma of the Foot
You may feel as if you have a rock or marble tucked into your…

How Your Gait Can Cause Back Pain
Back pain is a common health problem that can significantly impact…

The Connection Between Ankle Pain and Back Pain
When you think about ankle pain in Austin, TX, you might not…
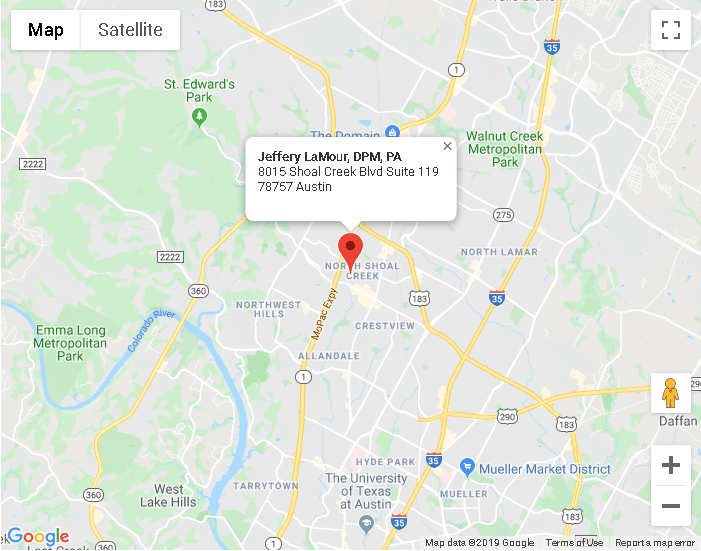
Austin TX
8015 Shoal Creek Blvd Suite 119Austin, TX 78757
Phone: (512) 451-3668
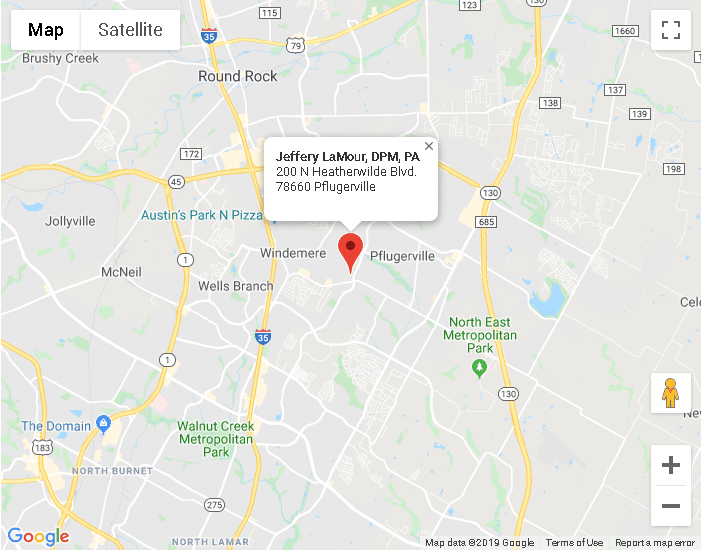
Pflugerville TX
200 N Heatherwilde BlvdPflugerville, TX 78660
Phone: (512) 451-3668