The Connection Between Diet and Toenail Fungus
Toenail fungus is a common problem. And it’s extremely hard…

Keeping Feet Healthy This Summer
Podiatrists see more patients in summer than any other time.…

Do I Have a Foot Corn or a Plantar Wart? How to Tell the Difference
It’s not entirely uncommon for people to confuse corns and…

Are Plantar Warts Painful?
Plantar warts are growths that show up on the bottom of your…

Three Types of Arthritis That Can Severely Affect Your Feet
Did you know that arthritis can affect your feet? It can. In…

Does a Pinched Toe Mean I Have Hammertoe?
Pinched toes are a relatively common occurrence, and they can…

3 Signs Your Bunions Are Causing Your Foot Pain
Bunions are more than an annoyance for many people. Of course,…

I Think I Have Foot Fungus - How Can I Get Treatment?
Foot fungus is a problem that can affect athletes as well as…
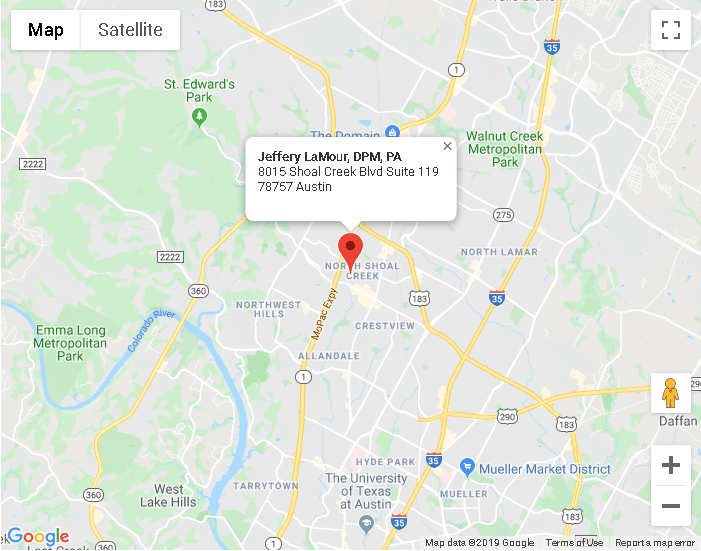
Austin TX
8015 Shoal Creek Blvd Suite 119Austin, TX 78757
Phone: (512) 451-3668
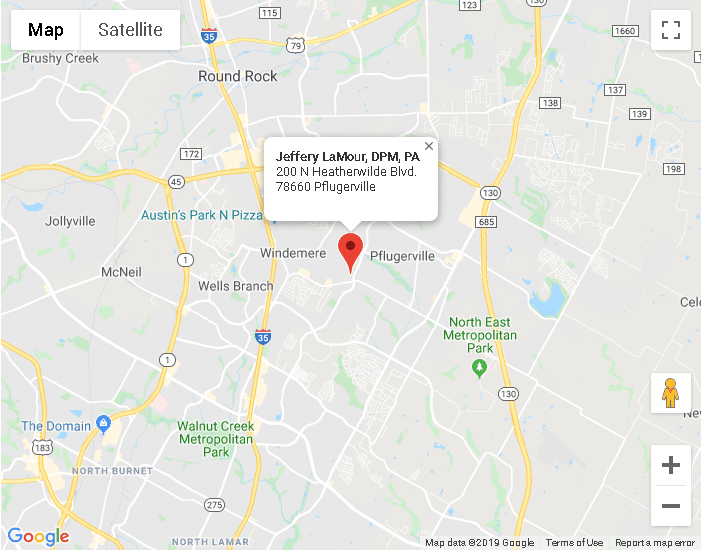
Pflugerville TX
200 N Heatherwilde BlvdPflugerville, TX 78660
Phone: (512) 451-3668