Top Three Best Treatments for Ankle Injuries
Ankle pain can bring your world to a full stop, regardless of…

Is Plantar Fasciitis Keeping You Off Your Feet? We Can Help
Plantar fasciitis in Austin TX is a common problem that causes…

What Does Diabetes Do to My Feet?
Do you have diabetes? If you do, you could be at risk for foot…

5 Tips to Avoid Ingrown Toenails
Ingrown toenails is a condition where the top of the nail grows…

Why Does Only One Toe Hurt After Running?
Running injuries may be common, but not all of them are explainable.…

3 Things to Know About Morton's Neuroma
The nerves in your foot can change over time, usually due to…

You Enjoy Wearing High Heels? 5 Tips to Save Your Feet
High heels can be hard on your feet, but your foot doctor in…

What Is a Neoplasm in Your Foot?
A neoplasm is a type of tissue that can form inside the foot.…
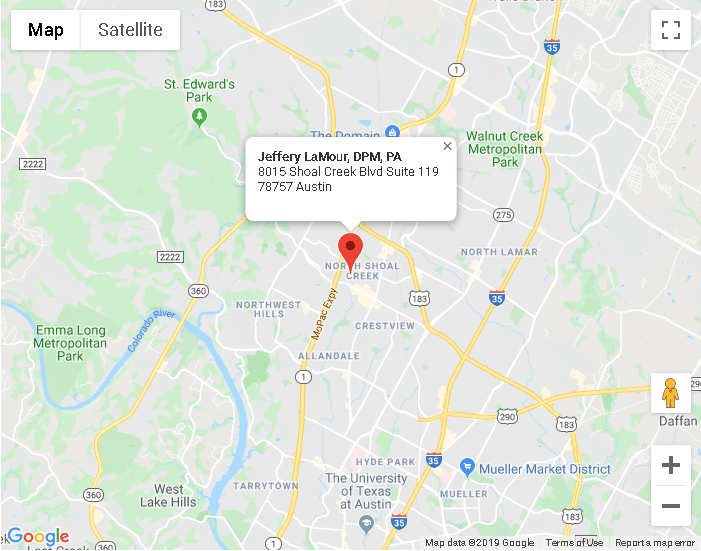
Austin TX
8015 Shoal Creek Blvd Suite 119Austin, TX 78757
Phone: (512) 451-3668
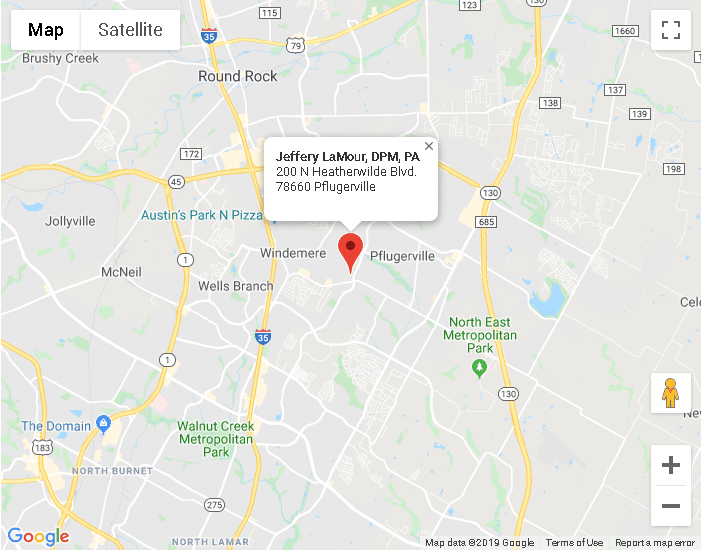
Pflugerville TX
200 N Heatherwilde BlvdPflugerville, TX 78660
Phone: (512) 451-3668