3 Important Facts About Blood Circulation in Your Foot
Most people know that the body will try to protect the core first.…

Custom Orthotics vs Store Bought Orthotics: The Wrong Choice Could Cost You
Do your feet hurt? There are plenty of reasons for foot pain,…

You Broke Your Toe Now What?
Oh no, you broke your toe, now what? A broken toe could be serious,…

What Is Fibrous Scar Tissue?
When your body is injured, whether it’s from a fracture or…

Plantar Fasciitis vs. A Heel Spur: How to Tell the Difference
Heel spurs and plantar fasciitis both cause heel pain, which…

When NOT to Use OTC Shoe Inserts
The companies that make over-the-counter (OTC) shoe inserts also…

3 Grades of Sprained Ankles: What to Know
The terms sprained and twisted when applied to the ankle can…

What Are the Most Effective Treatments for Athlete's Foot?
Estimates of athlete’s foot are relatively high in the US,…
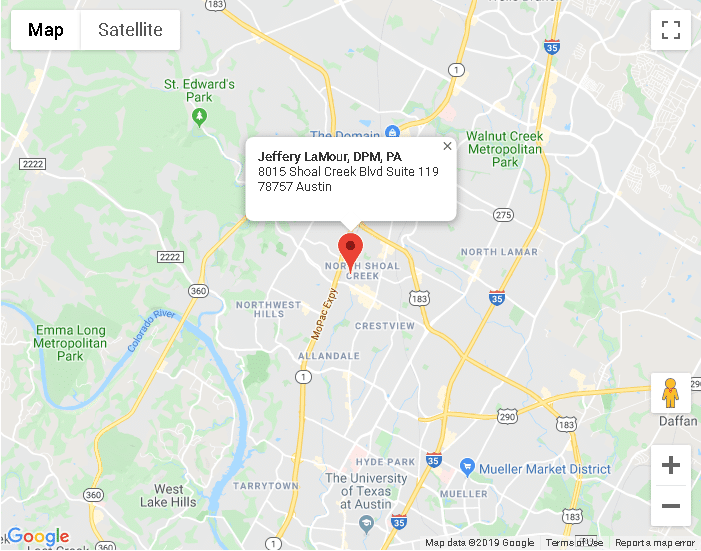
Austin TX
8015 Shoal Creek Blvd Suite 119Austin, TX 78757
Phone: (512) 451-3668
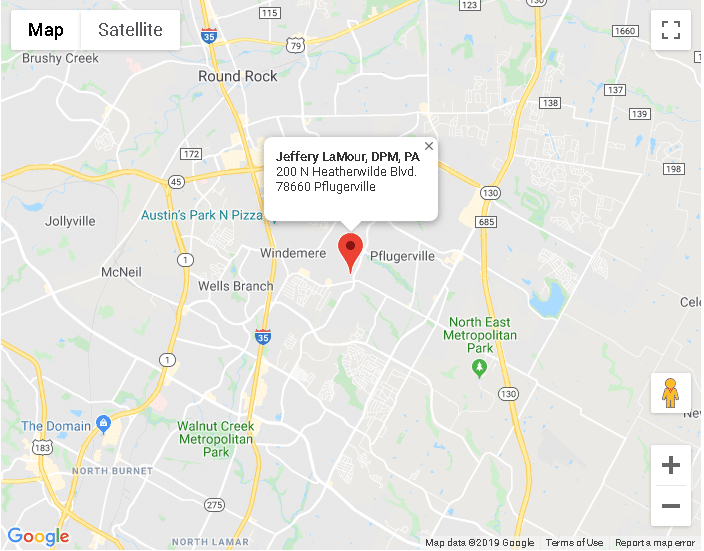
Pflugerville TX
200 N Heatherwilde BlvdPflugerville, TX 78660
Phone: (512) 451-3668