Treatment Options for Ingrown Toenails
Is your toe unusually sore? It may be that you have an ingrown…

What Can Be Done for Hammertoe?
Does your second, third, or fourth toe have an unusual bend at…

3 Signs of a Granuloma
A granuloma annulare in Pflugerville, TX is a type of rash that…

Can You Get Psoriasis on Your Feet?
Psoriasis is an itchy skin condition that's caused by an unusual…

Is Bunion Surgery Worth It?
Bunion surgery is one of the treatment options that your podiatrist…

Tips for Treating Calluses at Home and When To Call a Podiatrist
While performing weight-bearing activities (e.g., walking), the…

Should I Wear Over-the-Counter Shoe Inserts?
If you have foot discomfort, you may be tempted to pick up a…

Finding Shoes When Dealing With Bunions
If you have bunions, you know how difficult it is to find comfortable…
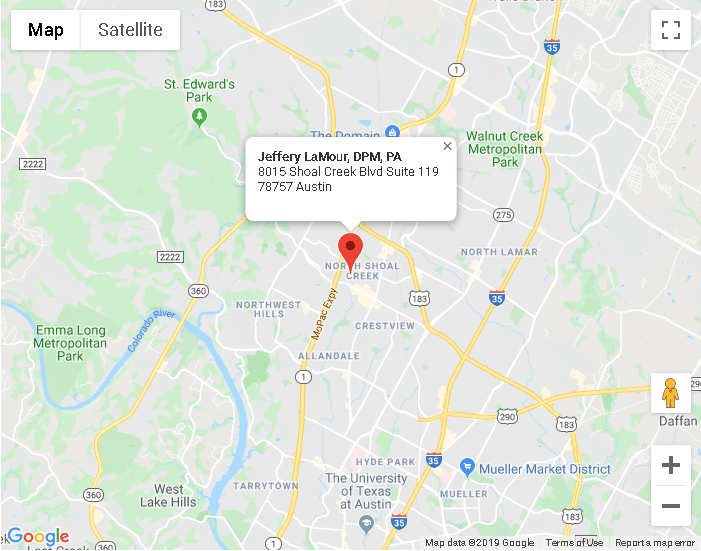
Austin TX
8015 Shoal Creek Blvd Suite 119Austin, TX 78757
Phone: (512) 451-3668
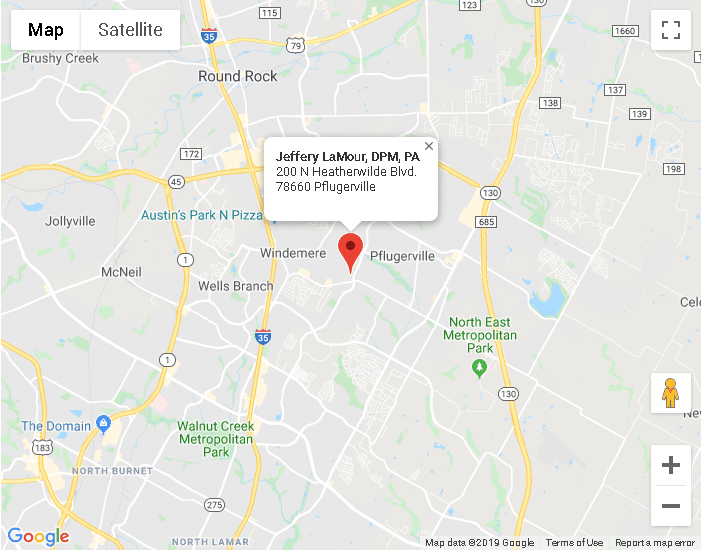
Pflugerville TX
200 N Heatherwilde BlvdPflugerville, TX 78660
Phone: (512) 451-3668