Common Symptoms of Neuroma of the Foot
Oftentimes, patients that visit a podiatrist for diabetic foot…

What to Look For in a Running Shoe
Running can be a great way to stay in shape. But if you are wearing…

Back Pain? The Problem Could be With Your Feet
If you suffer from chronic back pain and it hasn’t responded…

What Causes Bunions?
The malformation of the joint of the big toe is commonly known…

Is Toenail Fungus Dangerous?
It may seem odd to have to visit a podiatrist in Austin, TX for…

What Causes Ingrown Toenails?
Ingrown toenails occur when a sharp corner of your nail rubs…

Do I Have to Only Wear Flat Shoes Forever?
If you have had trouble with your feet, your Austin, TX podiatrist may…

Achilles Tendinitis: Signs and Symptoms
Your Achilles tendon is the band of tissue that connects the…
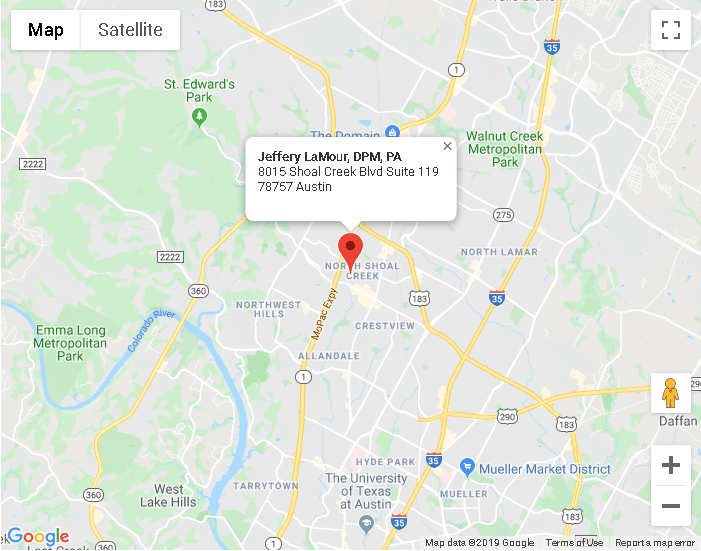
Austin TX
8015 Shoal Creek Blvd Suite 119Austin, TX 78757
Phone: (512) 451-3668
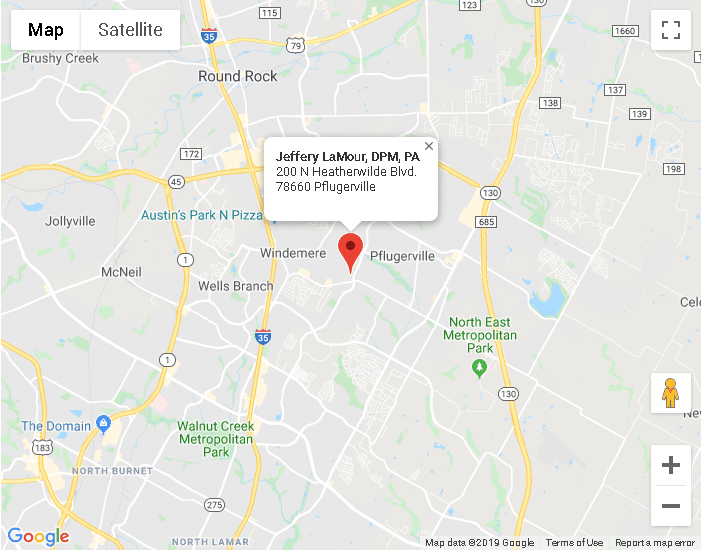
Pflugerville TX
200 N Heatherwilde BlvdPflugerville, TX 78660
Phone: (512) 451-3668